Adjustment Reason Codes are used by insurance companies to explain adjustments, patient responsibility and denials on the Explanation of Benefits (EOB). Prior to reviewing this article, the user should understand how to post a payment. See ERA - Electronic Remittance Advice - ERA Tab article for details. To view the reason codes on the EOB, navigate to Billing | ERA. Locate the payment from the list and select “View EOB” under the Action drop-down options at the end of the row. 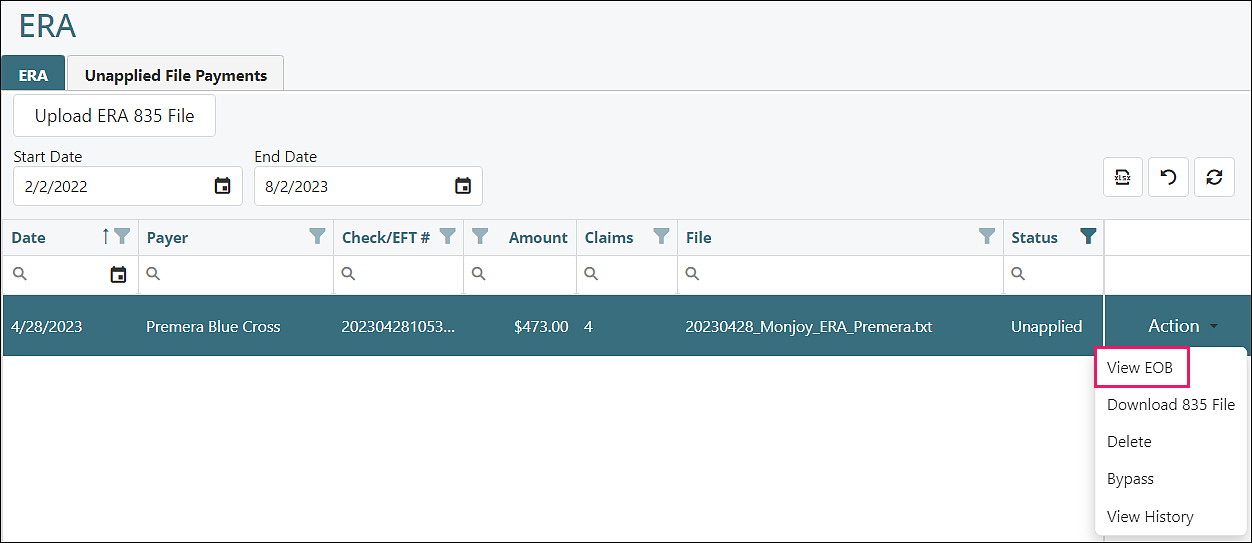
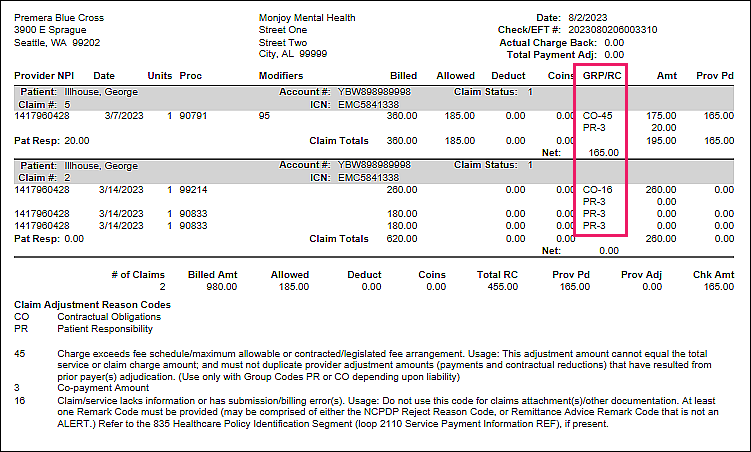
A new tab opens showing the EOB. The adjustment reason codes will be displayed in the GRP/RC column.
The adjustment reason codes are also located on the ERA files that are imported into Valant. To view the ERA file, navigate to Billing | ERA. Selecting the ERA and clicking Next in the bottom righthand corner will display the ERA. The arrow to the left of each individual payment will expand and display the adjustment reason codes from the insurance company.
Reminder: Users can review ERAs by selecting adjustment reason codes. Clicking the arrow to the right of the Select field displays selections determined by adjustment reason codes in the ERA.
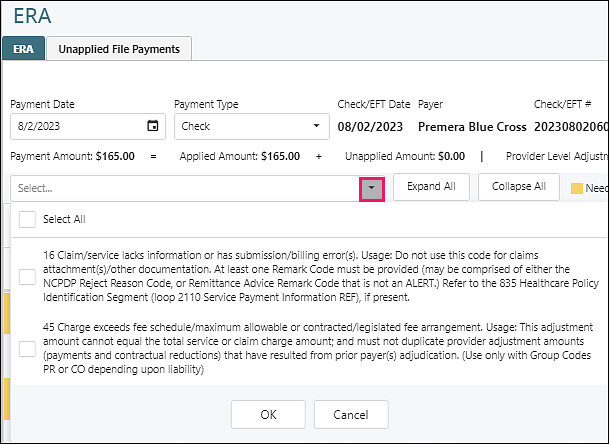
Adjustment Column Headers
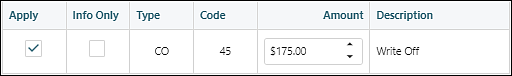
- Apply: checking this box will post the adjustment amount to the associated date of service in View/Edit charges when the payment is processed. The box is checked as a default for CO and PI type but can be unchecked and the amount listed will not be applied when the payment is applied.
- Info Only: checking this box will not apply the adjustment amount but will provide the explanation of the reason code on a transaction line in View/Edit charges. (40 characters maximum)
- Type (claim adjustment group codes)
- CO (Contractual Obligation): the amount the provider is contractually obligated to adjust from the claim.
- PI (Payer Initiated Reductions): used by payers when a reduction is made by the payer and the amount is not the patient’s responsibility.
- PR (Patient Responsibility): used to identify portions of the bill that are the responsibility of the patient. The following codes are not available for rules as they are built into core Valant billing functionality
- 1 = deductible
- 2 = copays
- 3 = coinsurance
- OA (Other Adjustments): used when CO or PR do not apply
- Code (claim adjustment reason codes): the number that represents the adjustment and description from the insurance company for an explanation of what has occurred with the claim. Codes are universal and set by X12 standard.
- Amount: the value that will be adjusted on the claim. This amount can be modified.
- Description: the explanation for the adjustment. Also pulled from X12 standard
Note: Some adjustment reason codes will default with a check in the Apply box. This means if the arrow to the right of each visit is not expanded and is not reviewed, the adjustment will occur when the payment is processed. In some scenarios, a practice does not want to automatically apply particular adjustment reason codes from particular payers. Valant offers rules to support these custom scenarios.
Adjustment Reason Code Rules
Practices can create adjustment reason code rules to prevent the automatic application of specific reason codes provided by the insurance company. To create adjustment reason code rules, navigate to Reference Data | Adjustment Reason Codes.
The Adjustment Reason Codes are automatically populated in Valant.
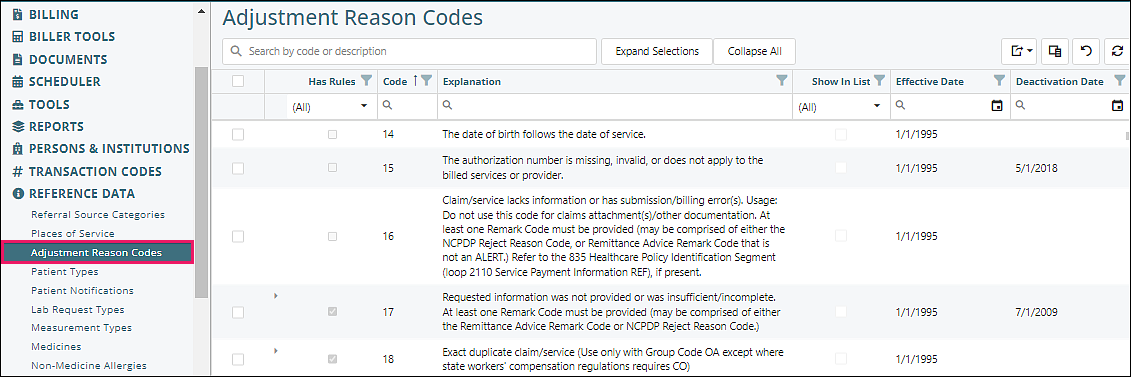
Top Fields
- Search: the code or words representing the code may be used to find the reason code
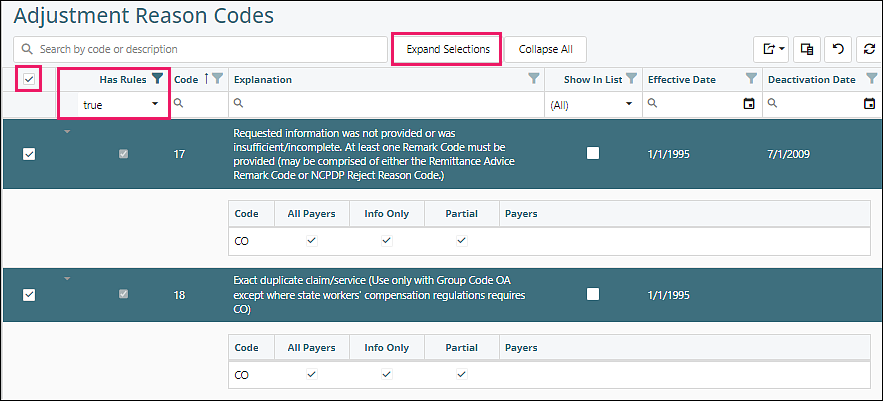
- Expand Selections: used to expand all selected adjustment reason codes with a rule
When a rule has been created the box in the "Has Rules" column will be checked. There will also be an arrow in the "Has Rules" column that indicates if the rule is expanded for a detail of the rule. Filter for "true", check top box on far left, then click Expand Selections.
- Collapse All: when multiple selections have been expanded, the collapse all button will close all that have been expanded.
Top Right Icons
![]()
 |
Export options |
| Exports the current view to an Excel spreadsheet | |
| Exports selected rows to an Excel spreadsheet | |
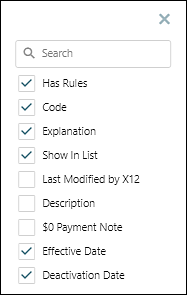
| Provides a list of columns that can be displayed. Unchecking or checking the box to the left of the desired column name will indicate if the column will be viewed on the screen. To optimize the view it is recommended that only columns used should be displayed/checked | |
| Removes all filters that have been set for any field | |
| Refreshes data if any changes were made |
Far Left Check Box: checking this box allows the use of the expand selections button at the top of the page if there are rules set up for this code
Columns
- Has Rule: indicates if the code has a rule
- Code: adjustment reason code
- Explanation: description of the adjustment reason code
- Show In List: allows the adjustment reason code to be visible while entering COB information on a payment that is posted manually
- Last Modified by X12: the date that the universal guidelines changed for this adjustment reason code
- Description: the default is ‘Other Insurance Adjustment’ displayed in View/Edit Charges and will appear on patient statements. This text can be customized on this page
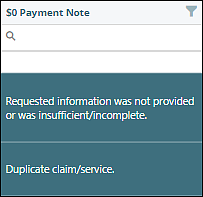
- $0 Payment Note: the note that will display in View/Edit Charges when the payment associated with this adjustment reason code is $0. This can be modified. The first 40 characters appear on patient statements. Examples in the below image:
- Effective Date – creation date of the adjustment reason code
- Deactivation Date - deactivation date for the adjustment reason code
Creating a Rule
The top part of the "Adjustment Reason" tab shows the information provided in the columns of the reason code list in the previous screen. The fields that are white can be edited.
To create a reason code rule, click on an adjustment reason code in the list.
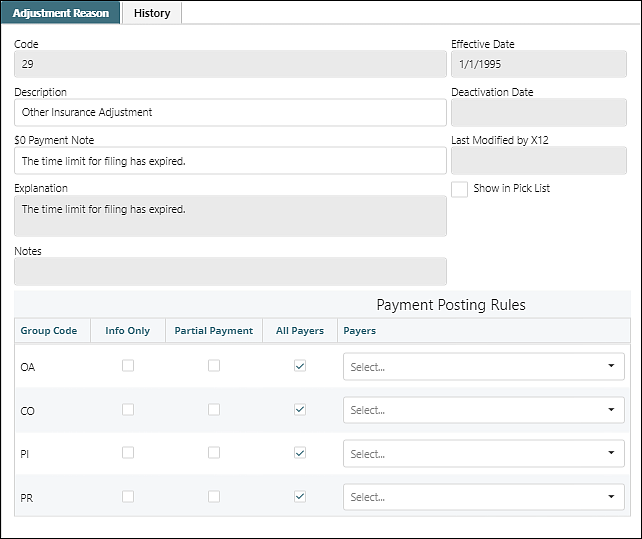
Payment Posting Rules Columns
- Group Code – all reason codes will start with one of the following types (claim adjustment group codes):
- CO (Contractual Obligation) is the amount the provider is contractually obligated to adjust from the claim.
- PI (Payer Initiated Reductions) is used by payers when a reduction is made by the payer and the amount is not the patient’s responsibility.
- PR (Patient Responsibility) is used to identify portions of the bill that are the responsibility of the patient. The following codes are not available for rules as they are built into core Valant billing functionality
- 1 = deductible
- 2 = copays
- 3 = coinsurance
- OA (Other Adjustments) is used when CO or PR do not apply.
- Info Only – Checking this box hides the information from statements, allows the information to be saved in View/Edit Charges, but will not apply to the adjustment. Any adjustments (for example: denials) with the info only box checked will not appear in COB information for secondary or tertiary payers.
- Partial Payment – this box will indicate additional responses are expected from the payer and will not forward any remaining balance to the next responsible party (insurance 2/3 or the patient). The payment will remain in this state until the next insurance payment or denial is posted to this charge. This means a claim file for the secondary or tertiary insurance will not be queued after this ERA is posted. In other words, the charge in View/Edit Charges will not be yellow.
- All Payers – allows the rule to be for every insurance company
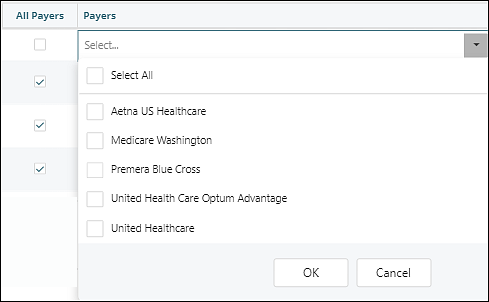
- Payers – if the “All Payers” box is unchecked, the payer box can be used to select the insurance companies that the rule needs to apply to.
Scenarios for Using Rules
Adjustment Reason Code 17 - Requested information was not provided or was insufficient/incomplete. At least one Remark Code must be provided (maybe comprised of either the Remittance Advice Remark Code or NCPDP Reject Reason Code.)
This code will be on an ERA when the insurance company requested information and they have not received it.
Adjustment Reason Code 18 - Exact duplicate claim/service (Use only with Group Code OA except where state workers' compensation regulations require CO)
This code will be on an ERA when the insurance company’s records show they have already processed a claim from this provider on this date.
Adjustment Reason Code 29 - The time limit for filing has expired.
This code will be on an ERA when the insurance company believes that the claim was not submitted within the terms of the contract.
In each of these scenarios, making a rule that does not adjust the claim, holds the balance in the insurance responsibility, and provides the information for the denial, will prevent the user from having to manually do it on every claim in an ERA. The user can then research the claim appeal if necessary or make the adjustment if the research concludes that payment is not warranted by the payer.
Example Rule Setup
Navigate to Reference Data | Adjustment Reason Codes. Select code 17.
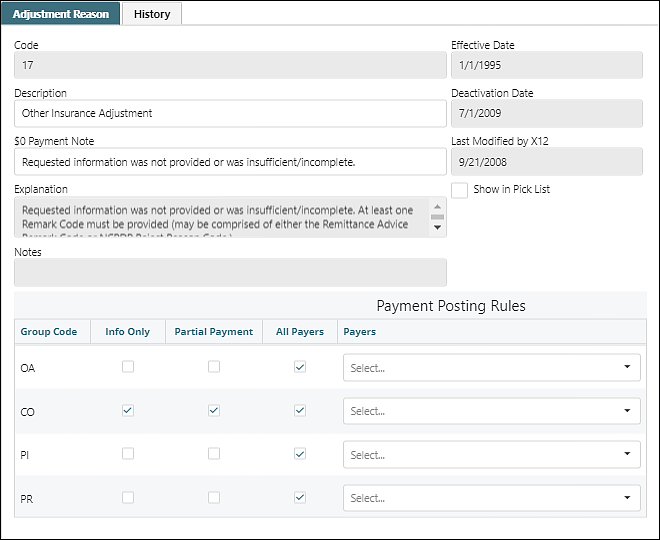
The functionality of the rule is created under the section "Payment Posting Rules".
- Next to the desired Group Code check the Info Only box (no adjustment will be made) and the Partial Payment box (the balance will remain in the current insurance and not be forwarded to the next payer).
- Leaving the box All Payers checked will apply this rule to all insurances. Unchecking this box will require selection of the specific payers.