Valant offers several settings and configurations to enhance the billing workflow by validating that required data is present before a charge is finalized. The following settings and features can be used independently, so the practice can choose the validation options that meets their needs.
Navigate to Persons & Institutions | Practice | Preferences tab
Users with Admin permissions will be able to see these settings
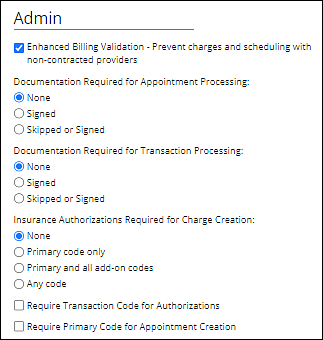
Enhanced Billing Validation - Prevent charges and scheduling with non-contracted providers
In Persons & Institutions | Insurance Companies | select an Insurance Company | Provider Information tab, the providers are checked “Contracted?” with insurance companies by default, but the box can be unchecked.
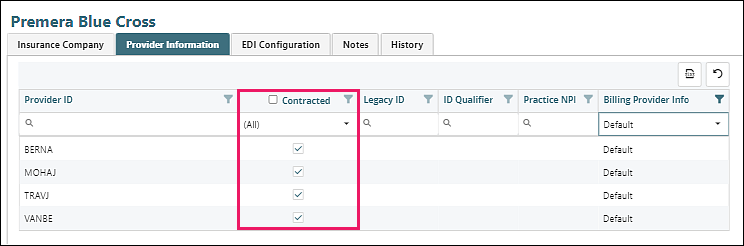
When "Enhanced Billing Validation - Prevent charges and scheduling with non-contracted providers" is checked, users will not be able to schedule patient appointments or process appointments through the PTQ if a provider is not contracted.
-
If the patient has no primary insurance when the appointment is scheduled, the appointment will fail validation. Meaning the appointment cannot be saved on the calendar. You will be able to save the appointment without a transaction code if you are awaiting insurance information for the patient.
- Note that patients who are paying out of pocket will need an Insurance 1 with the insurance type “Self Pay” selected.
- If the appointment provider is not contracted with the patient’s insurance, but the incident-to-supervisor in the appointment is contracted the patient’s insurance, the appointment will pass validation.
- If the appointment provider is not contracted with the patient’s primary insurance but is contracted with the patient’s secondary insurance, and the primary insurance has the checkbox “Bill Secondary as Primary when Provider is Not Contracted” checked, the appointment will pass validation. (Secondary will be the only insurance billed in the transaction).
Documentation Validation
Some practices require providers to sign their clinical documentation before the billing charge is finalized and eligible for claim submission. Two settings can enforce this requirement at different points in the charge creation process.
- Documentation Required for Transaction Processing – appointments can be recorded without complete documentation, but charges cannot be processed out of the Pending Transactions Queue without signed (or skipped) documentation. The documentation column in the PTQ shows the documentation status.
- Documentation Required for Appointment Processing – appointments cannot be recorded without signed (or skipped) documentation. Practices that enable this setting typically also enable the Receipt Book feature to allow staff to collect patient payments without recording the appointment.
Procedure Code Validation
The procedure code list in Fee Schedules includes a column called “Valid”. This field is used to indicate what procedure codes per insurance company can be billed. When scheduling users will receive a warning that if they schedule an appointment with a procedure code that is not checked as “Valid”. This is a soft-stop as the user will be able to save the appointment. However, the transaction will not be processed through the PTQ without a valid procedure code.
Pending Transaction Queue
When transactions in the PTQ are validated or processed, a window appears with their status. Items that do not meet validation requirements cannot be processed through the PTQ, and an error message lists the validation failures. Items that meet validation requirements can be processed through the PTQ and charges will be created. See the Pending Transactions Queue (PTQ) article for more information.
Validation Chart
Validation Type |
Scheduler |
PTQ |
Provider Contracted |
Hard Stop |
Hard Stop |
Procedure Code |
Soft pop-up warning |
Hard Stop |
Documentation Status |
Optional Hard Stop |
Optional Hard Stop |