When a payment is received from the insurance that is not automatically imported as an ERA (for example, a check received in the mail or an electronic fund transfer), a manual entry needs to occur through the Apply Insurance Payment function. To complete the entry, information from the Explanation of Benefits (EOB) is necessary.
To access "Apply Insurance Payment", click Billing | Apply Insurance Payment
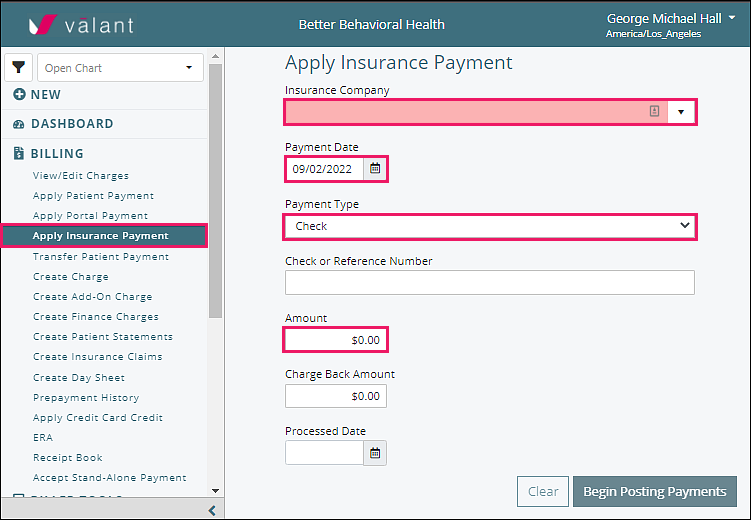
Enter the Insurance Company from the drop-down list, the Payment Date, the Payment Type from the drop-down list, and the Amount.
Optional Fields
Check or Reference Number: enter the check number, EFT number, or other tracking number used by the practice
Charge Back Amount: noted on EOB (when insurance company recoups money previously paid), if amount entered in this field, a screen opens to select the patient from which the insurance company is recouping money. Select the claim indicated on the EOB, enter the amount in the Apply column. Click Continue to proceed.
Processed Date: enter date of EOB when the patient has a secondary insurance and COB (coordination of benefits) information is needed for the secondary claim.
Note: When a "Charge Back Amount" is entered, the payment "Amount" should not be changed as the system will calculate the distribution of the charge back appropriately.
If Charge Back Field is Populated
The Charge Back process is described in the Charge Backs article.
Post Payments with no Charge Back
Click Begin Posting Payments in order to find the patient and charge to assign this payment. Choose a patient to apply all or part of an insurance payment. Only patients with charges that are payable by the chosen insurance company will appear on this list.
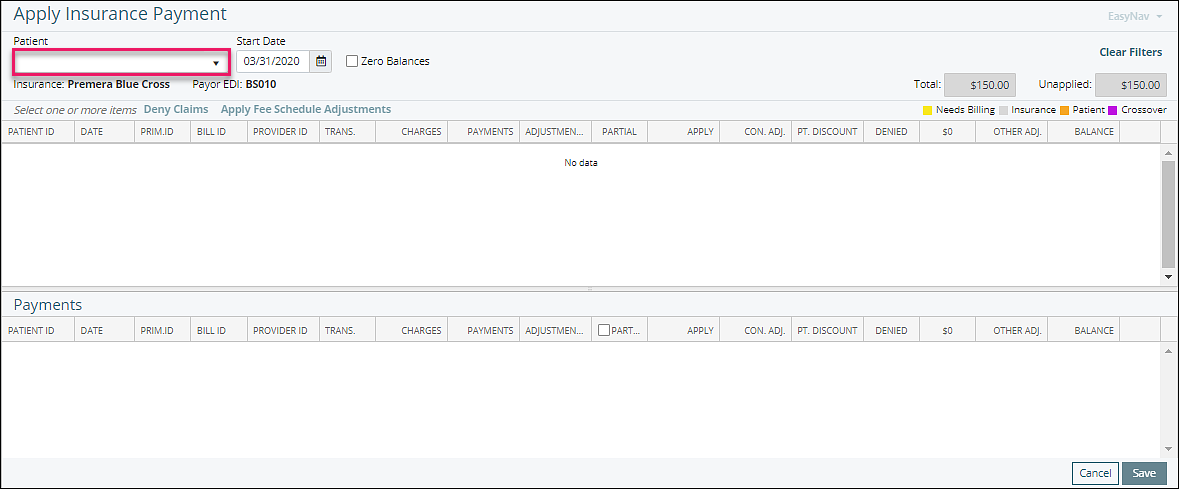
Note: If your patient does not show up, check Person & Institutions | Patients. Select the patient and go to the Ins tab to make sure the insurance is correct for that patient.
Identify the claim for the appropriate date of service
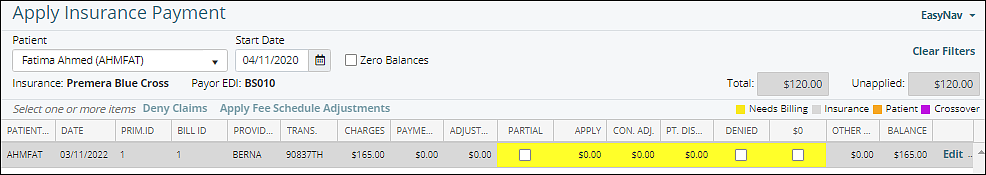
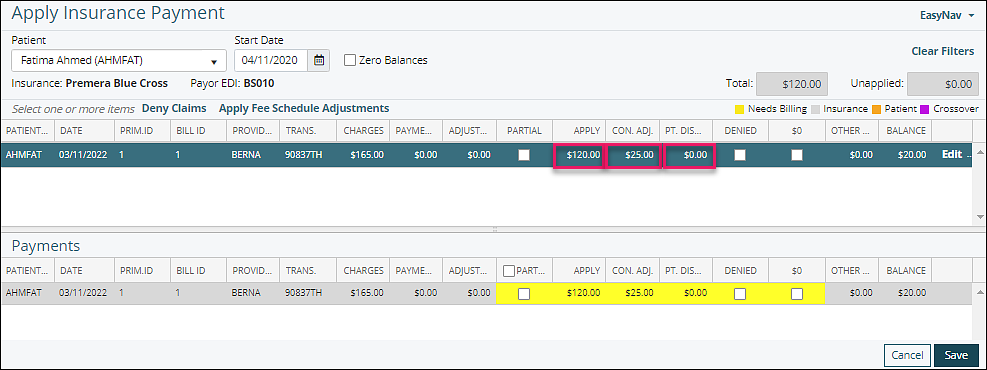
Use the EOB payment and adjustment amounts to enter the information for the appropriate date of service.
Apply: amount being applied to the transaction as stated on the payer EOB
Con. Adj.: contractual adjustment amount being applied to the transaction as stated on payer EOB.
Note: If Fee Schedules are set up for the payer, then the Con. Adj. automatically populates which assists with making sure the payment is according to contract. This amount can be manually adjusted in the Con. Adj. field.
Pt. Discount: amount of discount being applied to the transaction from the practice
Optional checkboxes:
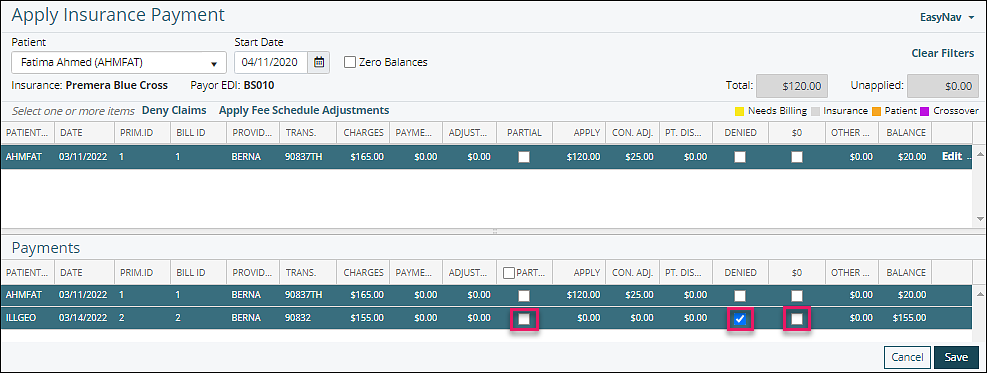
Partial: indicates the payment is a partial payment. The remaining balance will stay with this payer
Denied: use when insurance payment is denied
$0: use when no insurance payment is made, but no denial is given. Example: Patient deductible amount.
Additional information can be added to a specific payment entry, click on "Edit"
A window will appear, opening the Patient Payment Details window, that will allow a Note to be entered for information already in place for the payment details. The notes will show up on the patient statement.
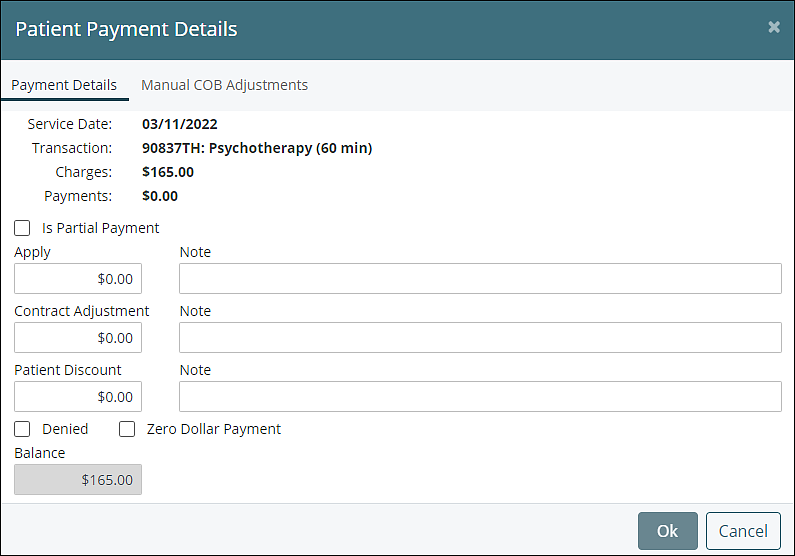
The Manual COB Adjustments tab provides additional information about the payment. See Manual COB article for more information on this process.
When applying a payment to a specific patient is completed, another patient can be selected. All completed actions will be listed in the bottom half of the screen and will replicate the information on the EOB.
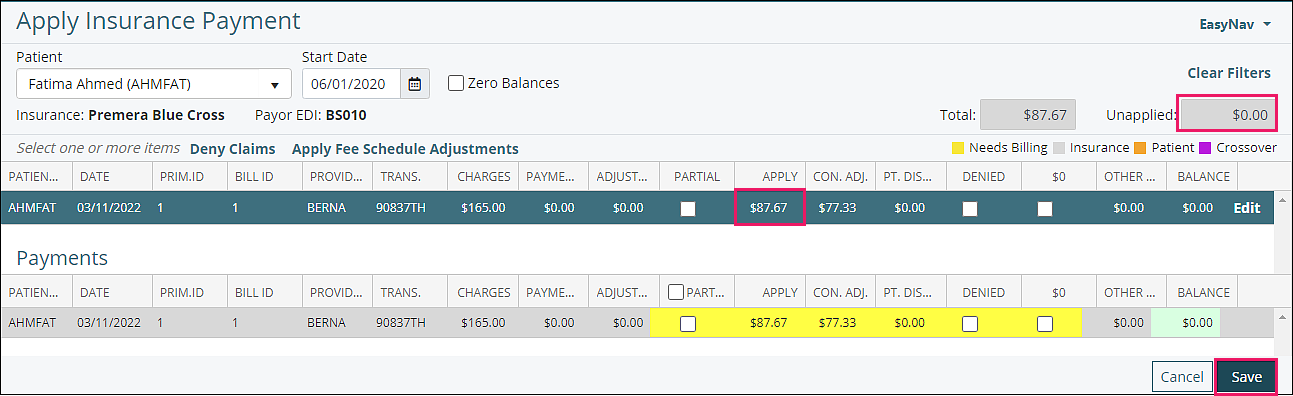
The unapplied field indicates the amount of the payment that remains to be applied. Payment application cannot be saved until the entire payment amount has been applied and the unapplied field reads "$0.00".
Click Save
After saving the payment the details can be viewed in "View/Edit Charges". Posting an insurance payment will also move balance to patient responsibility for those with Auto bill patient checked in Persons & Institutions | Patient | Demo tab.