Reporting is knowledge, and knowledge provides you with the information you need to analyze your practice. Valant provides you with an abundance of reports to use daily, weekly and monthly. These sections will provide you with some basic reports that you will want to begin running as soon as you start billing in Valant.
Pending Insurance Claims
The Pending Insurance Claims Report is a Billing Report in System Reports that is used to see which claims are in Valant and pending insurance submission. Charges that have been created and set to be billed to an insurance payor will show on this report. This will include charges that show as yellow in View/Edit Charges. The filters on the report allow you to filter by specific Insurance Payor, Facility, Patient, Provider or Responsible Payer (Primary, Secondary, or Tertiary). Apply filters and click Preview.
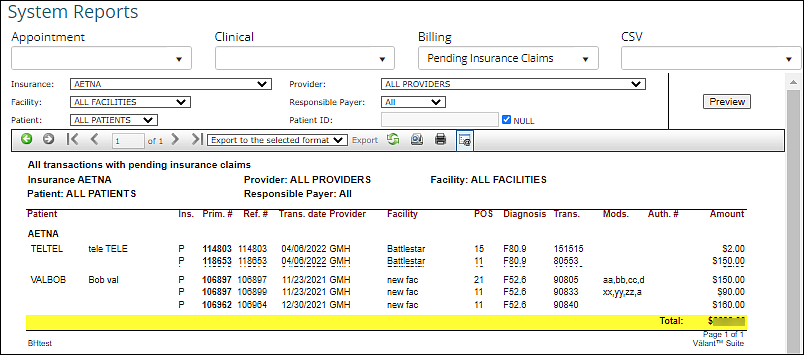
This report is useful to find claims that are pending insurance submission, and can also be useful to run before submitting claims to see which claims are going to be submitted. If a claim is appearing on this report and not being send when creating a batch of claims for electronic claim submission it is always good to check and make sure that the EDI Payor ID is added for the insurance company. This is a common issue when practices are trying to send a claim for a newly added insurance company.
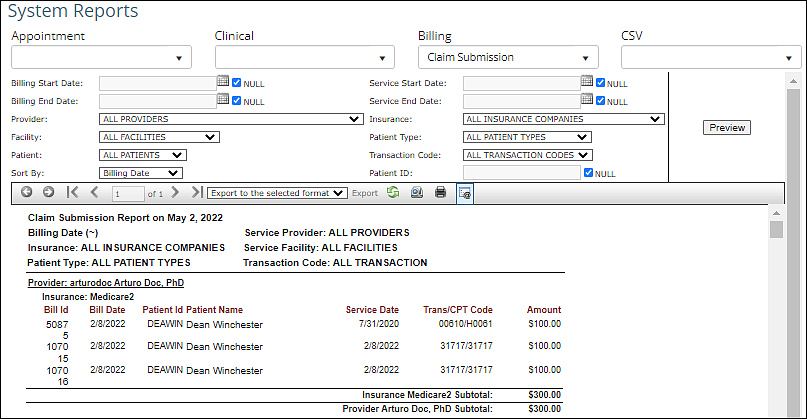
DeleteClaim Submission
The Claim Submission Report is a Billing Report in System Reports that is used to see which claims are in Valant that have been submitted to insurance. Charges that have been created and billed to an insurance payor will show on this report. This will include charges that show as grey in View/Edit Charges. The filters on the report allow you to filter by specific Billing and Service Dates, Provider, Facility, Patient, Insurance, Patient Type, or Transaction Code. The report can be sorted by Billing Date or Date of Service. Apply filters and click Preview.
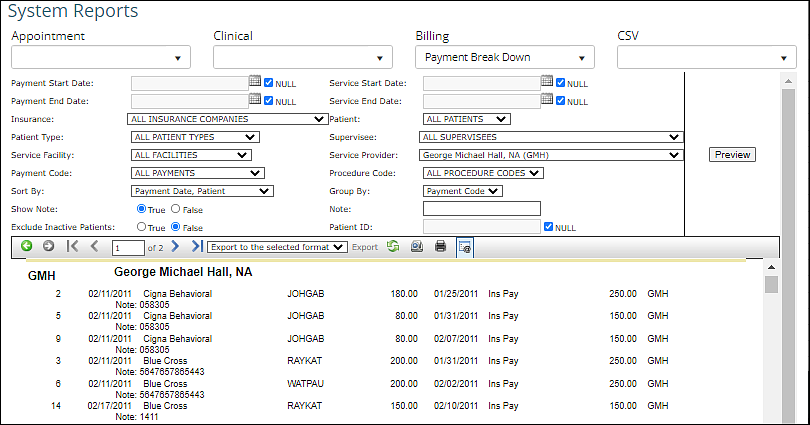
Payment Break Down
The Payment Break Down Report is a Billing Report in System Reports that allows your practice to review payment details. The filters on the report allow you to filter by specific Payment Date, Insurance, Patient Type, Facility, Payment Code, Service Date, Patient, Supervisee, Service Provider, or Procedure Code. Information can be sorted by any option in the Sort By; drop down field. The report can currently be grouped only by Default (Date) or Payment Code. Apply filters and click Preview.
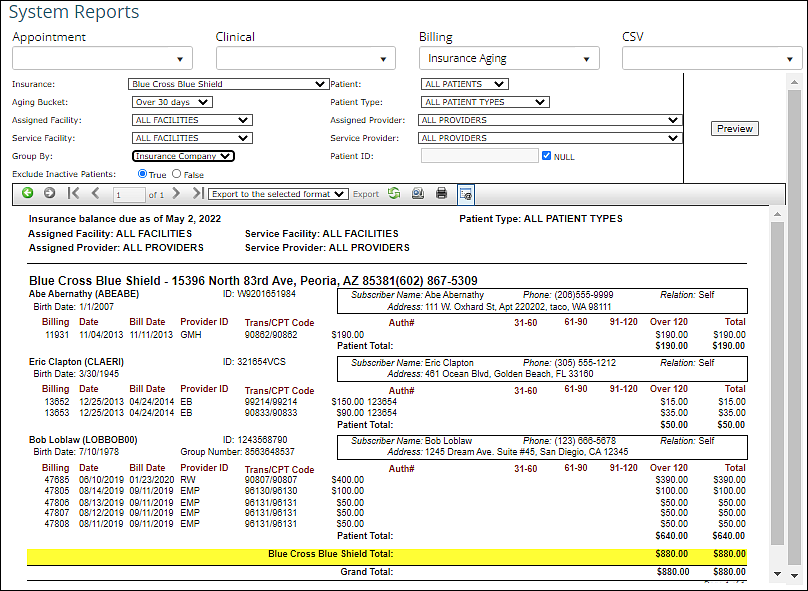
Insurance Aging
The Insurance Aging Report is a Billing Report in System Reports that allows your practice to review claims that have been submitted to an insurance payor, but are awaiting response. Practices should print this report monthly and use it to follow up on outstanding insurance claims. The filters on the report allow you to filter by specific Insurance, Aging Bucket, Facility, Patient Type, or Provider. The report can be grouped by Insurance Company, Facility, or Provider. Apply filters and click Preview.
Patient Aging
The Patient Aging Report is a Billing Report in System Reports that allows your practice to review outstanding patient responsibilities where a patient payment has not been posted. Practices should print this report monthly and use it to follow up on outstanding patient balances. The filters on the report allow you to filter by specific Patient, Patient Type, Facility, Aging Bucket, or Provider. The report can be grouped by Patient or Provider. Apply filters and click Preview.
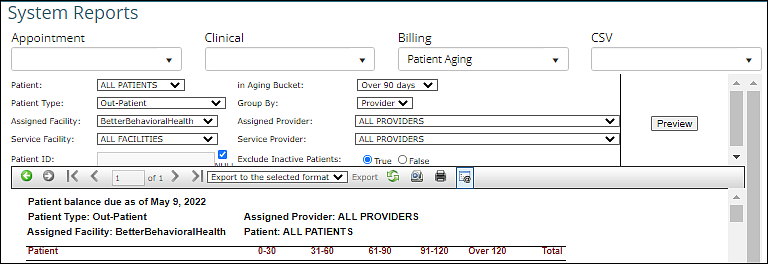
Each dated line indicates a statement has been printed and sent to the patient via mail or portal.
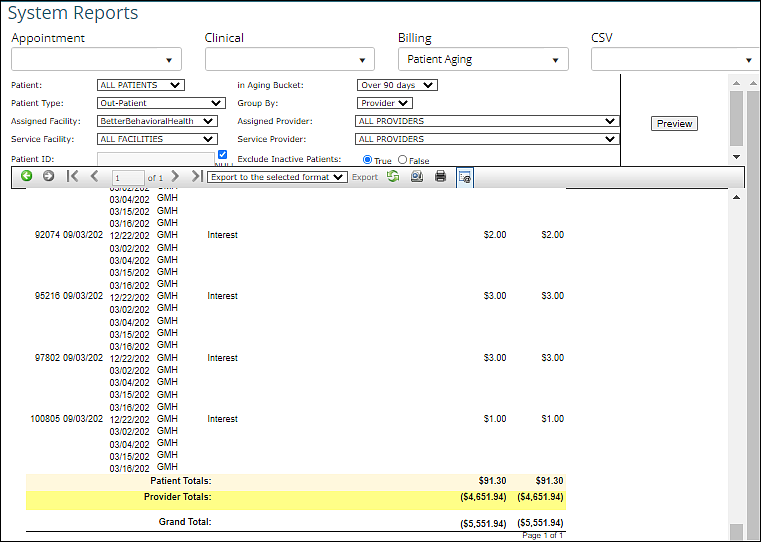
Note: The aging process for a charge begins when it is marked as printed in a patient statement.
DeleteTransactions
The Transactions Report is a Billing Report in System Reports that allows your practice to review transactions by a date range. Practices can run and export this report to review and sort the detail behind each transaction. The filters on the report allow you to filter by specific Patient Type, Provider, Supervisee, Facility, Patient, or Transaction Code. The report can be grouped by Patient, Provider, or Date. Apply filters and click Preview.
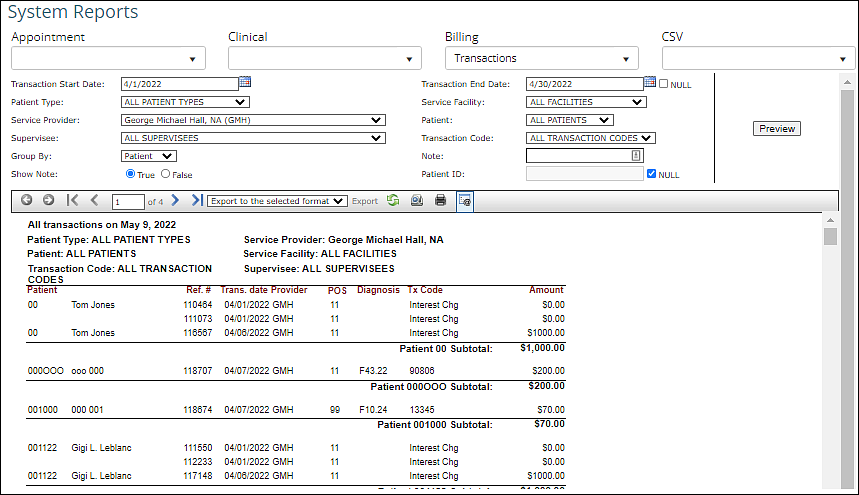
Note: If NULL is checked by the Transaction End Date field, a specific end date cannot be selected, and the report will show transactions through the current date.
DeleteIntegrated CC Transactions
This requires the Report Center module.
The Integrated CC Transactions report is a report that is available in the Report Center that shows the user a list of transactions with integrated credit card processing in Valant IO. The report can be found under Reports | Report Center | Integrated CC Transactions.
The report has two grouping options:
Transactions: this grouping will show all Elavon transactions. The date range filter used is the Transaction Date Range.
Transactions & Charges: this grouping displays the dollar portion of the transaction that was applied to the associated charge.
This report will post details about transactions and include transaction date, amount, and transaction status. If the report is grouped by "Transactions & Charges", the credit card payments applied to the charge will appear below the transaction line in a grey row. If the report is grouped by "Transactions", the credit card payments applied to the charge will not show on the report. The Patient ID is a hyperlink that can be clicked to go directly to View/Edit Charges for the patient. The Tx Origin (a column to the far right of the report) will identify if payment was made by the practice (Auto CC) or patient portal (Online Bill Pay). The report shows the last four numbers of the card.
In the shaded area above the report data, there are a number of filters available to narrow down the list of payments if desired.
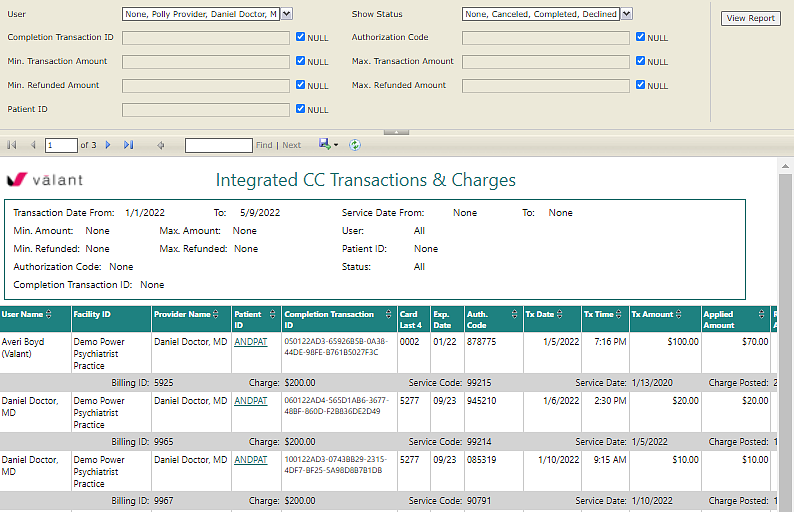
Note: This report will only show transactions from Valant IO. Also, this report may show credit card credits of negative amounts, in the event there is a failed credit being applied to a card.
Delete