Practices that have an integrated clearinghouse like Waystar or Change Healthcare can use Valant to check patients' insurance eligibility. Practices should make sure their payors are enrolled payors for eligibility checking at the clearinghouse level and make sure that the Eligibility ID is in place for the insurance company in Valant.
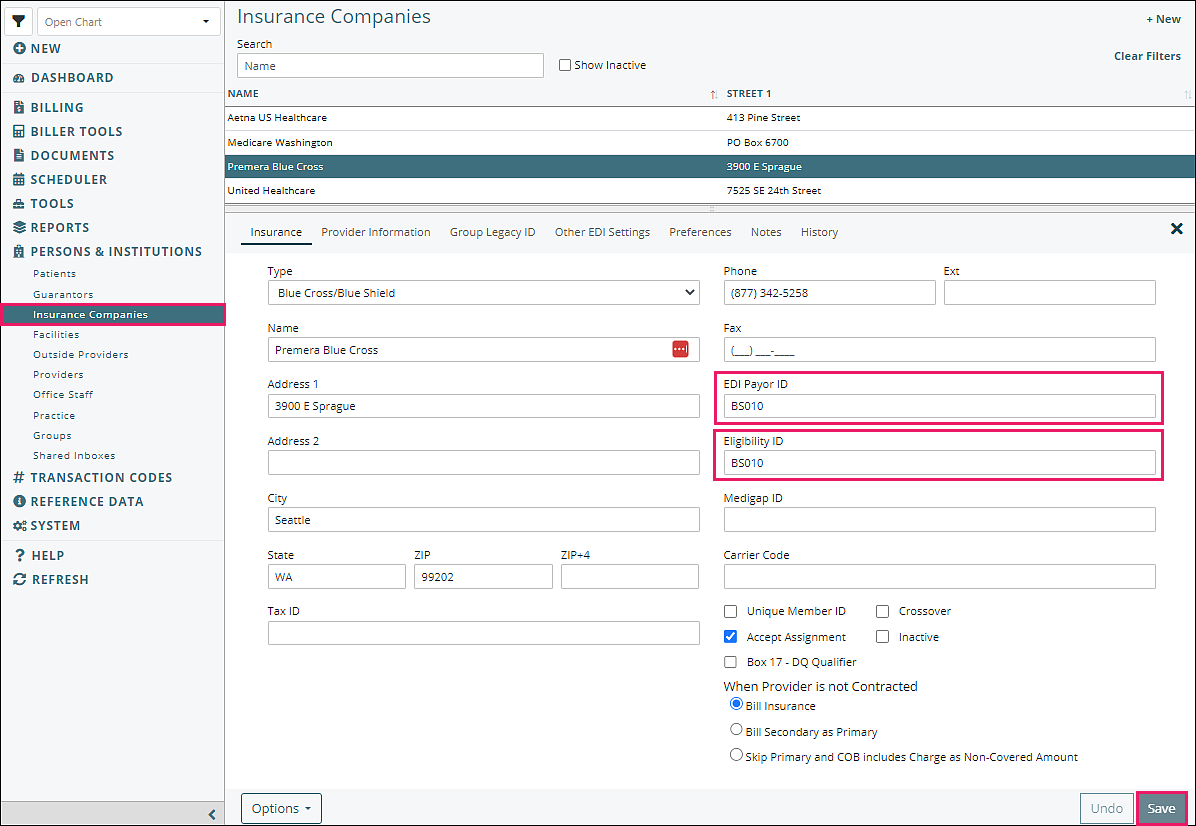
Each insurance company must have EDI Payor ID and an Eligibility ID supplied by Waystar. For ChangeHealthcare the EDI Payor and the Eligibility ID are the same. The following step will only need to be completed once in the setup.
- Navigate to Persons & Institutions | Insurance Companies from the left menu
- Select a payor and enter "EDI Payor ID" and the "Eligibility ID"
- Click Save
There are three places to run eligibility checks in Valant:
Patient's Insurance Tab
One way to run an eligibility check is from the Insurance tab of the patient information. This is used mostly when adding insurance for a new patient or updating insurance payors for a patient.
- Navigate to Persons & Institutions | Patients | select a patient | Ins tab
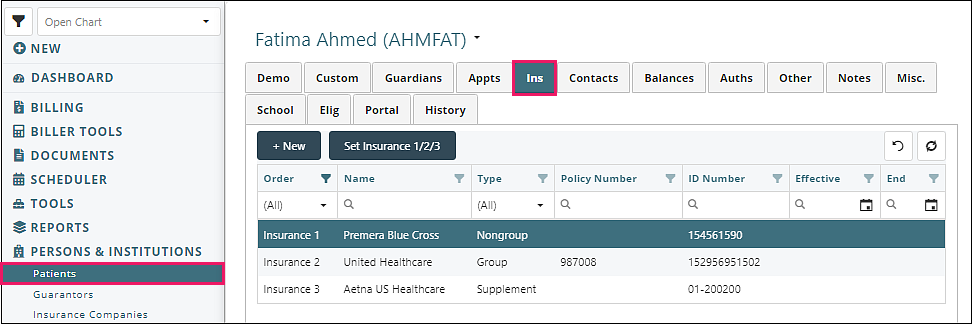
- Click on an insurance which opens the "Patient Insurance" window
- Click Check Eligibility
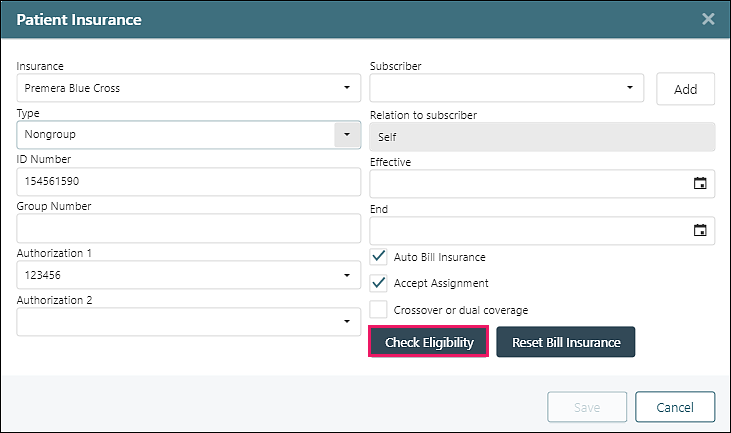
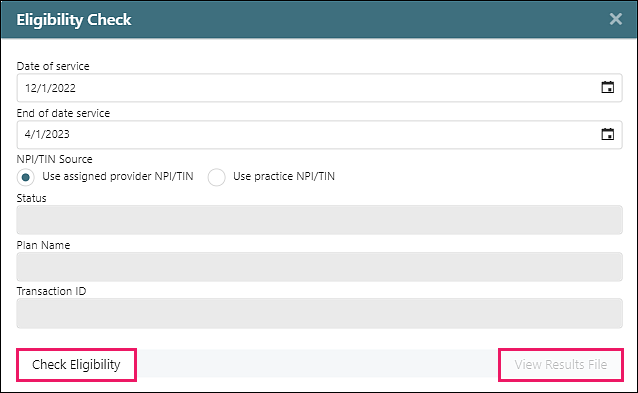
- This will opens the "Eligibility Check" window.
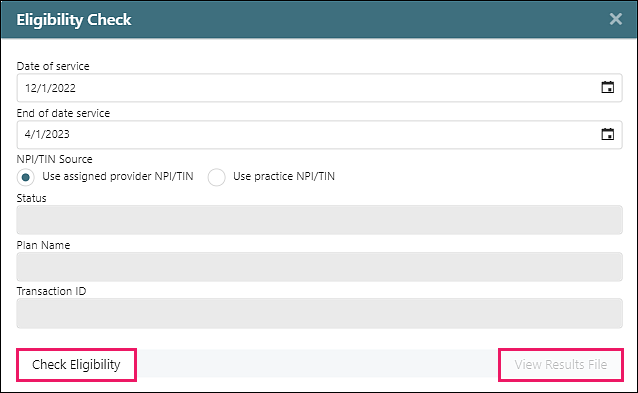
- Click Check Eligibility: the response from the payor will show in the window
- Click View Results File: a full results file can be viewed
Appointment
Eligibility Checking can be done from the appointment on the Dashboard or in the Scheduler. This is most useful when scheduling an appointment or before an appointment for a patient that already exists in the EHR. To check eligibility from the appointment:
- Right-click on an Appointment, click Check Eligibility
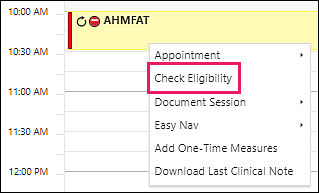
- This will open the "Eligibility Check" window
- Click Check Eligibility: the response from the payor will show in the window
- Click View Results File: a full results file can be viewed
Batch Eligibility Checks
Users also have the option of running Batch Eligibility checks to check insurance coverage for more than one patient at a time. Use case: checking a whole week's or day's appointments.
Click Biller Tools | Batch Eligibility Checking
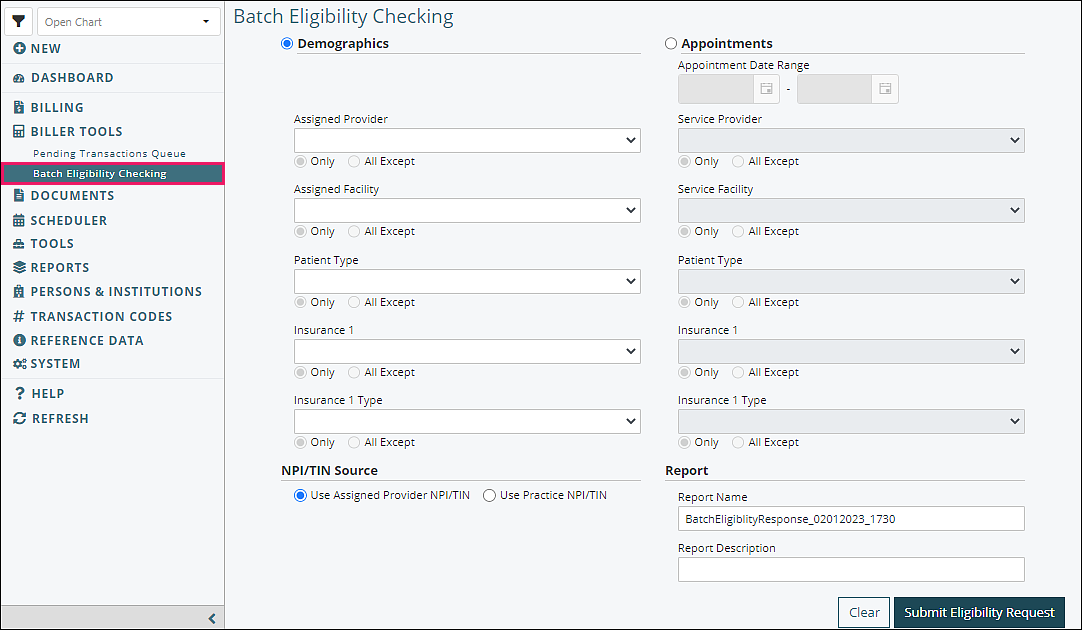
Information can be filtered either by patients' demographic information or by appointments scheduled in the calendar. The eligibility check itself is based on the patient’s primary insurance.
Filter by Demographics: only active patients whose demographics match the criteria will be included in the batch eligibility request.
- Assigned Provider Drop-down: filter the batch eligibility request by patients' assigned providers.
- Insurance 1 Drop-down; filter the batch eligibility request by patients' primary insurance.
- Insurance 1 Type Drop-down: filter the batch eligibility request by patients' primary insurance types.
Filter by Appointments: only patients with a scheduled appointment will be included in the batch eligibility request.
- Appointment Date Range: filter the batch eligibility request by appointment date.
- Service Provider Drop-down: filter the batch eligibility request by service provider.
- Service Facility Drop-down: filter the batch eligibility request by service Facility.
- Insurance 1 Drop-down: filter the batch eligibility request by patients' primary insurance.
- Insurance 1 Type Drop-down: filter the batch eligibility request by patients' primary insurance types.
Report Name: the name/title of the batch eligibility report as displayed in the Report Queue.
Report Description (optional): a description of the report which shows when hovering over the Report Name in the Report Queue.
Clear: clears all controls on the Batch Eligibility Checking Tab.
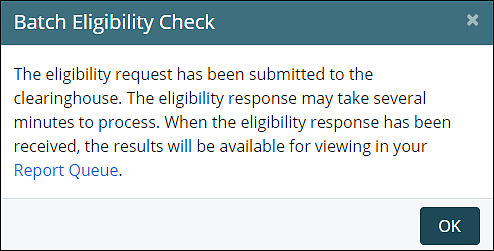
Submit Eligibility Request: sends the batch eligibility request to the partnered clearing house. When a response is received, the eligibility information is sent to a report that is accessed from Report Queue.
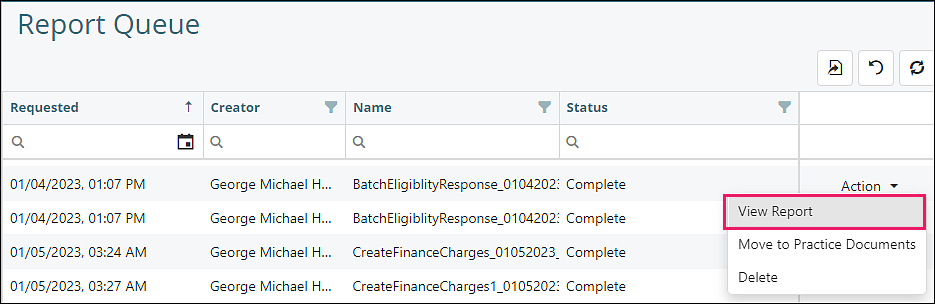
Click Tools | Report Queue
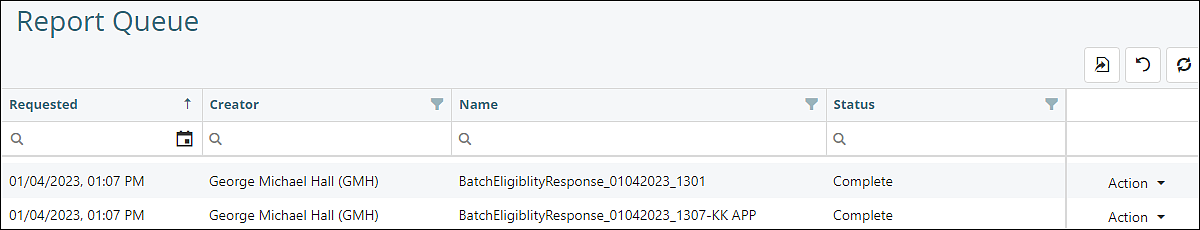
Click View Report from the Action drop down menu when the status is "Complete"
There are three sections of the report. The responses to these batch eligibility checks are only located in this report.
- Active Coverage: the patients listed here all received a valid response from the payer for the eligibility check. This response represents a general message from the payer and may or may not apply to the services specified in the appointment. In order to get complete details of the check, an individual eligibility check on the patient must be run from Persons & Institutions | Patients | Insurance 1 Tab.
- Inactive/Other: this area lists the patients which did not receive a valid response from the payer for the eligibility check. The reason for appearing here is that either the patient is not covered by that payer anymore or else another payer is responsible for covering the patient. The specific reason is supplied under the Response column next to the patient name
- Response Error: this section of the report is meant to display any response that came back due to a specific error. When possible, we include the error response from the payer in the report, however this might not always be available. It is advisable to run an individual eligibility check on the patient from Persons & Institutions | Patients | Insurance 1 Tab in order to get more details on any error messages which are unclear or require further information.